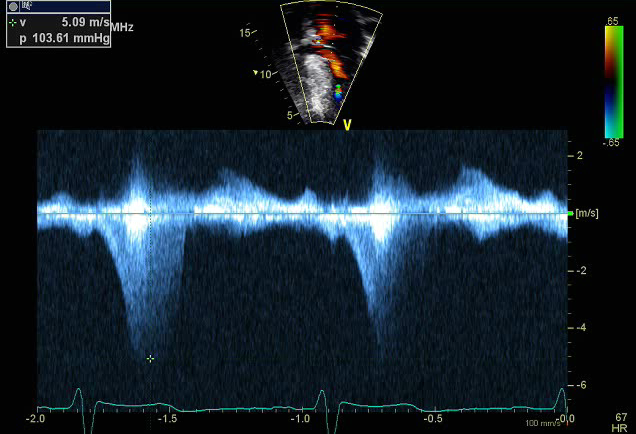
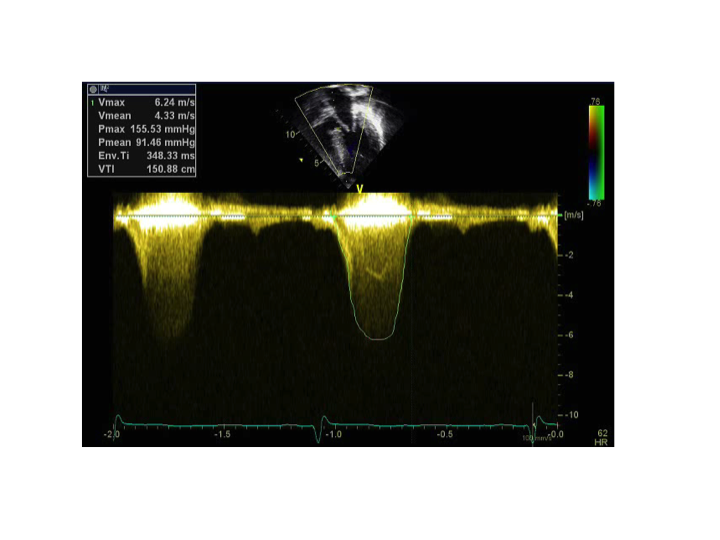
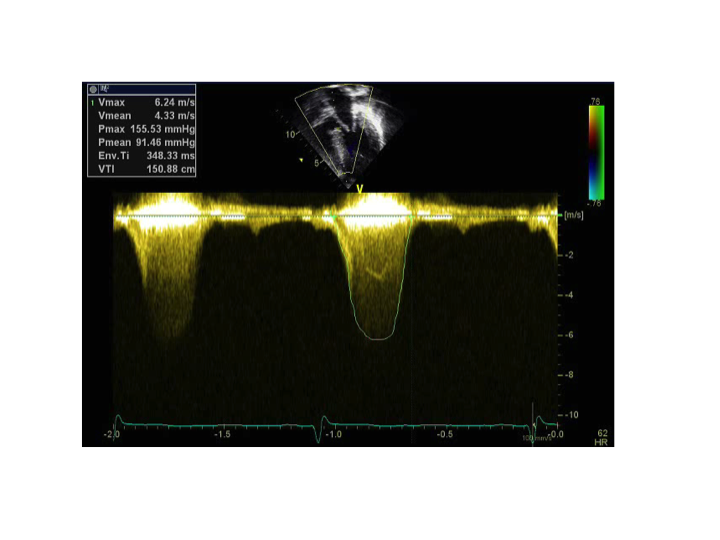
The apical 5 chamber view is a good view to assess for ventricular hypertrophy as well as left ventricular outflow tract obstruction. Obstruction to LV outflow is dynamic, varying with loading conditions and contractility of the ventricle. Increased myocardial contractility, decreased ventricular volume, or decreased afterload increase the degree of subaortic obstruction. Most recent studies that explain the mechanism of the outflow tract gradient in HCM emphasize that during ventricular systole, flow against the abnormally positioned mitral valve apparatus results in drag force on a portion of the mitral valve leaflets, which pushes the leaflets into the outflow tract. When a gradient is detected in the LV cavity, it is important to systematically exclude obstruction that is unrelated to SAM, including sub-aortic membranes, mitral valve leaflet abnormalities and mid-cavity obstruction, particularly when interventions to relieve LV outflow obstruction are contemplated.
For HCM, it is the peak instantaneous LV outflow gradient rather than the mean gradient that influences treatment decisions. Up to one third of patients with HCM will have obstruction at rest (defined as gradients ≥30 mm Hg). Another one third will have labile, physiologically provoked gradients (<30 mm Hg at rest and ≥30 mm Hg with physiologic provocation). The final one third will have the nonobstructive form of HCM (gradients <30 mm Hg at rest and with provocation). Marked gradients ≥50 mm Hg, either at rest or with provocation, represent the conventional threshold for surgical intervention if symptoms cannot be controlled with medications as significant outflow tract obstruction places patients at risk for ischemia, arrhythmias and sudden death.