Ventricular Septal Defect (VSD)
Overview
- A ventricular septal defect (VSD) is an abnormal communication between the right ventricle and left ventricle
- A VSD can be a single defect or multiple defects.
- A VSD can be found in isolation or associated with numerous variants of congenital heart disease (i.e.- TOF, truncus arteriosis, PA/IVS, transposition of the great arteries)
Epidemiology
- Approximately 20% of all CHD
- Incidence varies widely (5-50/100,000) and is likely underestimated
- secondary to spontaneous closure of smaller defects in fetal life and early postnatal life
- Slightly greater prevalence in females
Genetics
- Trisomy 21
- Trisomy 18
- Trisomy 13
- Holt Oram Syndrome
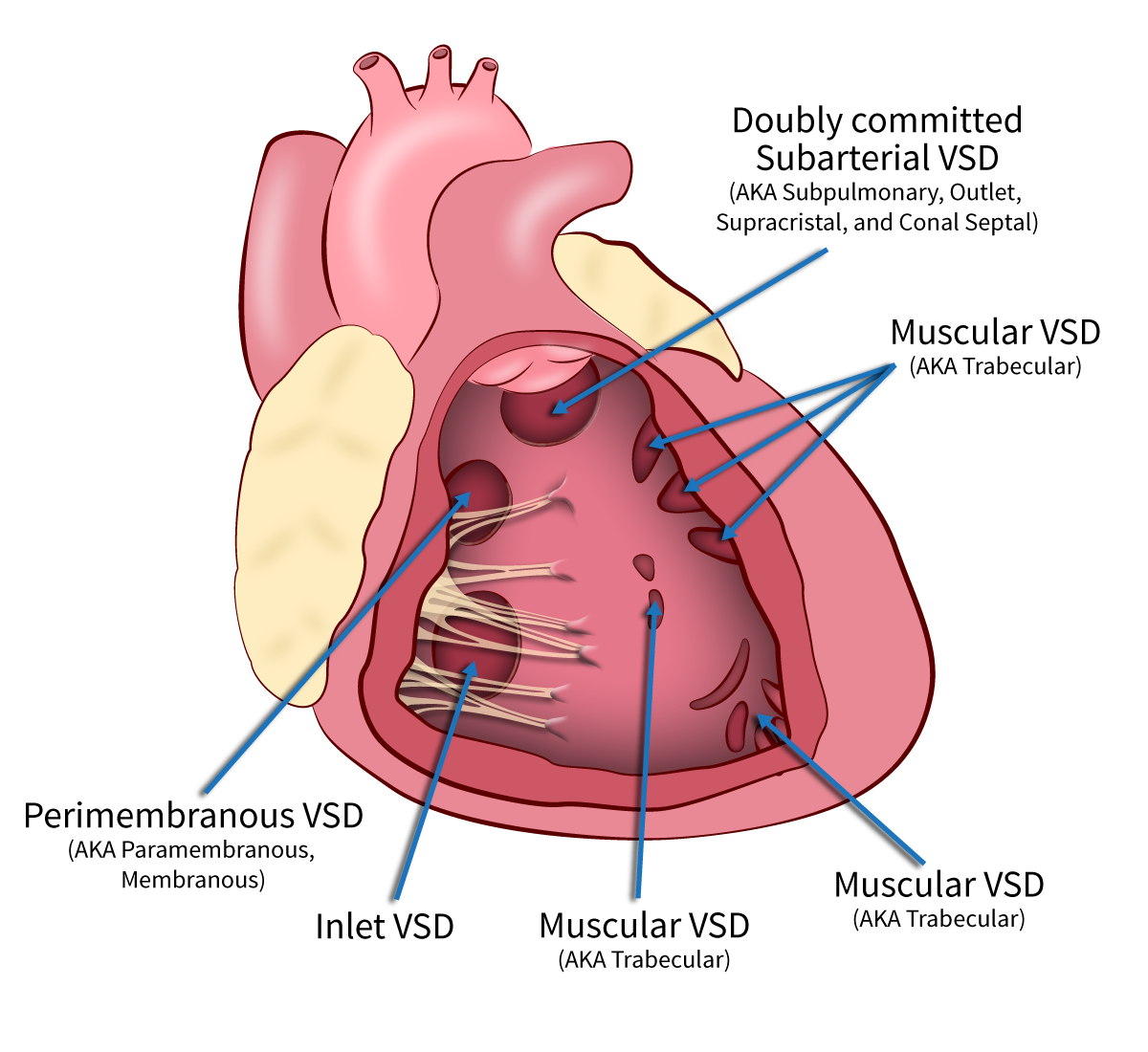
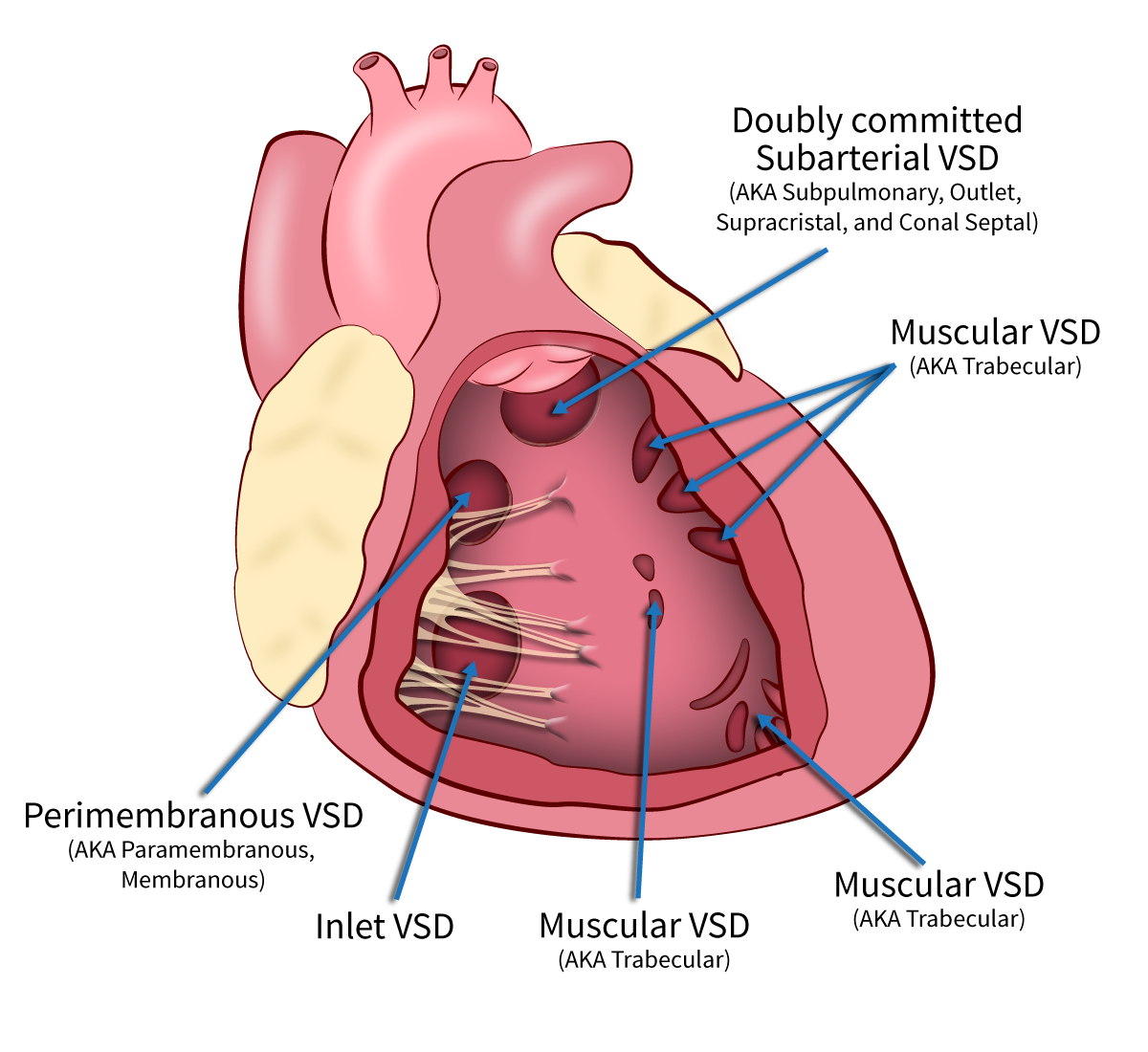
Types of VSDs
- Perimembranous (aka paramembranous, membranous) (80%)
- Muscular (aka trabecular) (5–20%)
- Doubly Committed Subarterial (aka conal septal, doubly committed juxta-arterial, subpulmonary, supracristal, outlet) (5–7%)
- Inlet (aka AV canal type) (5–8%)?
VSD Hemodynamics
- A VSD represents a pressure and volume load on the pulmonary vascular bed and results in increased pulmonary blood flow with subsequent increased pulmonary venous return to the left heart. Over time this can result in dilation of the pulmonary artery and left heart structures (left atrium, mitral valve and left ventricle). Depending on its size, a VSD can either be pressure restrictive (typically small defects) or pressure unrestrictive (larger defects).