- Fetal Complete Heart Block
- Fetal bradycardia with slow fetal ventricular rate is noted
- No current evidence of fetal Hydrops
- Fetal Complete Heart Block
- Fetal bradycardia with slow fetal ventricular rate is noted
- No current evidence of fetal Hydrops
- Fetal Complete Heart Block
- Short axis view of fetal ventricles
- Fetal bradycardia with slow fetal ventricular rate is noted
- Normal biventricular systolic function
- No current evidence of fetal Hydrops
- Fetal Complete Heart Block
- Fetal bradycardia with slow fetal ventricular rate is noted
- Moderate tricuspid regurgitation
- Mild mitral regurgitation
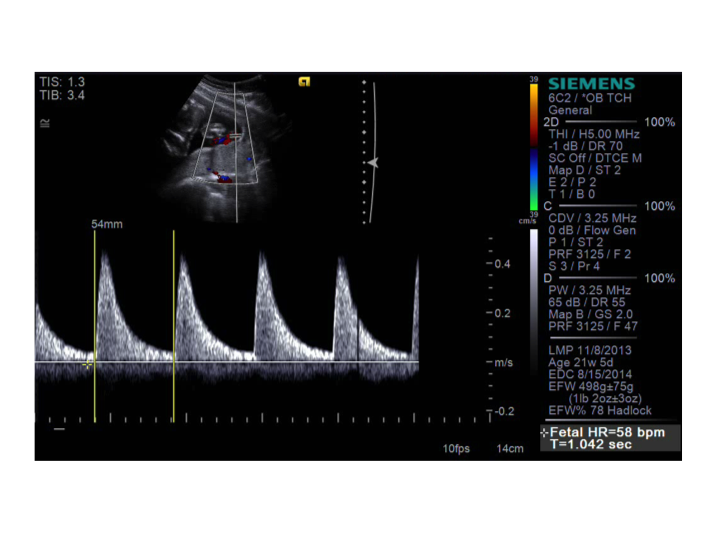
- Fetal Complete Heart Block
- Spectral Doppler in the umbilical artery in a fetus with complete heart block
- Fetal bradycardia at a rate of 58 beats/min
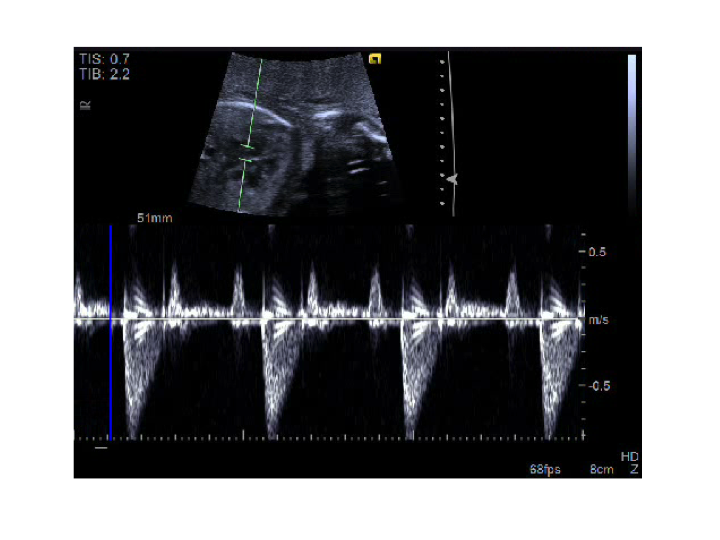
- Fetal Complete Heart Block
- Spectral Doppler capturing both mitral inflow and aortic outflow in a fetus with complete heart block.
- A slow ventricular rate is noted and faster atrial rate which is dissociated from the ventricular rate (2:1 complete heart block).
- A= atrial contraction (mitral inflow)
- V= ventricular contraction (aortic outflow)
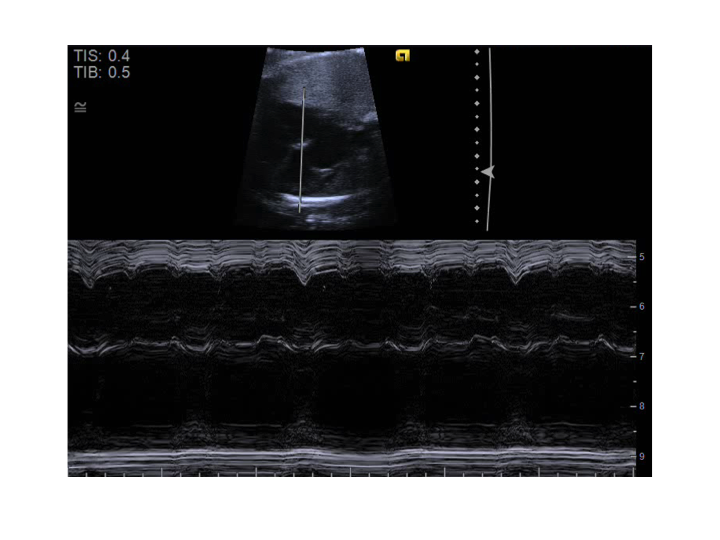
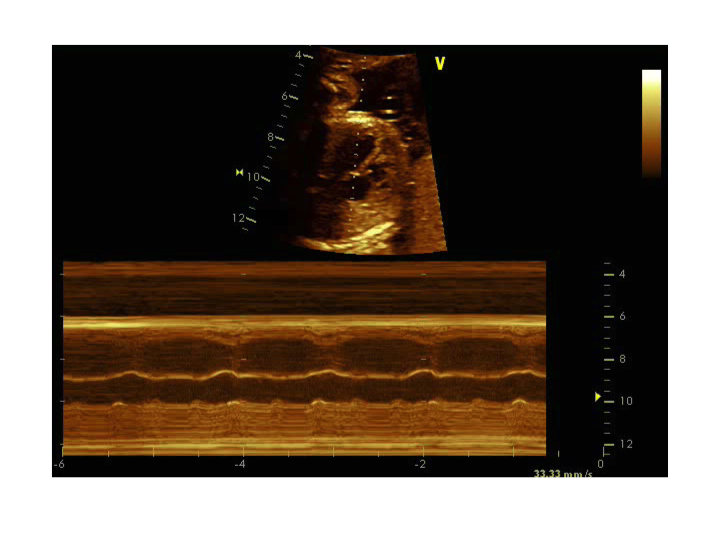
- Fetal Complete Heart Block
- M-mode through the right atrium and left ventricle in a fetus with complete heart block
- A slow ventricular rate is noted and faster atrial rate which is dissociated from the ventricular rate
- A= atrial contraction
- V= ventricular contraction
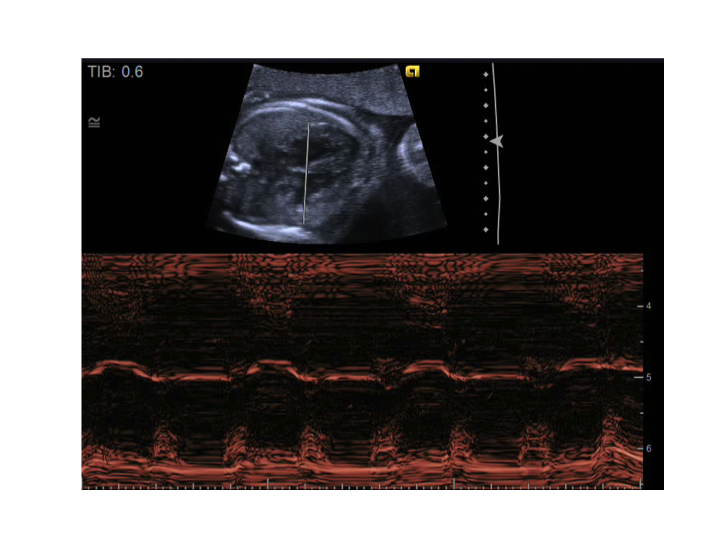
- Fetal Complete Heart Block
- M-mode through the right atrium and left ventricle in a fetus with complete heart block
- A slow ventricular rate is noted and faster atrial rate which is dissociated from the ventricular rate (2:1 AV block)
- A= atrial contraction
- V= ventricular contraction
- Fetal Complete Heart Block
- M-mode through the right atrium and left ventricle in a fetus with complete heart block
- A slow ventricular rate is noted and faster atrial rate which is dissociated from the ventricular rate
- A= atrial contraction
- V= ventricular contraction
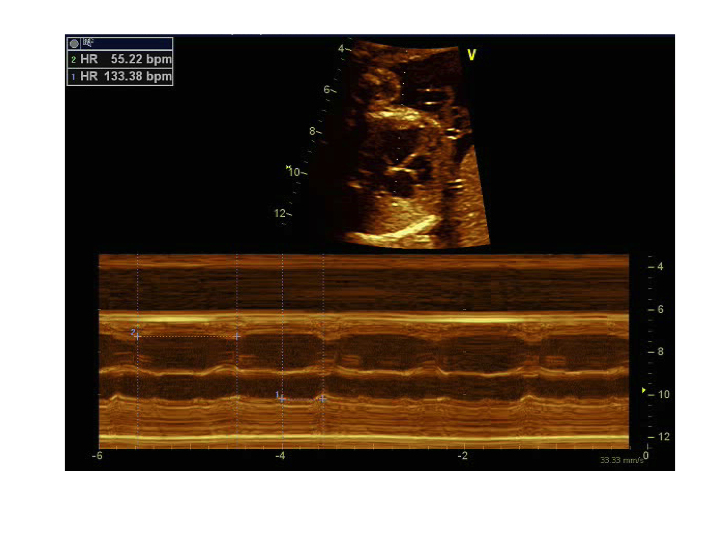
- Fetal Complete Heart Block
- M-mode through the right atrium and left ventricle in a fetus with complete heart block
- A slow ventricular rate is noted and faster atrial rate which is dissociated from the ventricular rate
- A= atrial contraction (atrial rate of 133 beats/min)
- V= ventricular contraction (ventricular rate of 55 beats/min)
Congenital Heart Block
Fetal congenital heart block (CAVB) is the presence of conduction system disease of any form, which is diagnosed on or before 28 days of life. The incidence of has been estimated from several studies to be about 1 in 22,000 live births. Although this is clearly an uncommon disorder, it may be associated with high mortality and morbidity and therefore requires a high index of suspicion for early diagnosis and aggressive therapy when appropriate. In somes cases, prenatal use of dexamethasone or the other maternal drugs (such as terbutaline), fetal pacing, or early delivery. There are no extensive data on the “appropriateness” of aggressive therapy, but our some papers suggest it may improve hydrops in the sickest fetuses.
Congenital heart block is frequently associated with underlying structural congenital heart disease (~40%). The most common forms of congenital heart disease associated with heart block include fetal heterotaxy (left atrial isomerism), often with an accompanying atrioventricular septal defect, as well as L-transposition of the great arteries. In cases where congenital heart disease is not present, congenital heart block is almost always secondary to maternal connective tissue disease (anti SSA/Ro antibodies). The cause of immune mediated CAVB is believed to be an inflammatory response with subsequent injury to the fetal myocardium and cardiac conduction system in susceptible fetuses secondary to circulating maternal antibodies.
Congenital heart block carries a high mortality in the presence of congenial heart disease (~70%) whereas the mortality in the setting of immune mediated CAVB is significantly lower (~19%).
Important Components of Fetal Echocardiogram:
- M-mode through atrium and ventricles (establish atrial rate and ventricular rate)
- Pulse wave Doppler of mitral inflow and aortic outflow
- Pulse wave Doppler interrogation of the superior vena cava and aora
- Assess for tricuspid or mitral regurgitation
- Assess chamber dimensions
- Assess right and left ventricular systolic function
- Fetal Hydrops (pericardial effusion, pleural effusion, ascites, skin/scalp edema)