Patent Ductus Arteriosus Aneurysm (DAA)
Monica Martin, RDCS (AE, PE)
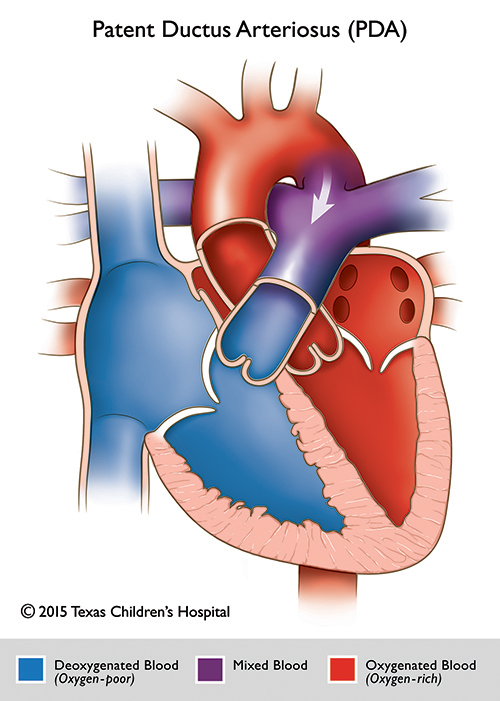
Patent Ductus Arteriosus Aneurysm (DAA) is a saccular or fusiform dilatation of the ductus arteriosus. Typically, the aneurysm presents as a large, thin walled, saccular dilatation of the ductus arteriosus often ending as a small tortuous PDA on the pulmonary side. The Internal diameter is usually equal to or larger than the transverse arch or descending aorta. A ductal aneurysm can be either congenital or acquired, as a complication of surgical closure of a patent ductus arteriosus.
The most common age for a ductal aneurysm is less than 2 months, however, it may be seen in children and adults as well. DAA was once considered a rare defect with significant complications including; compression of surrounding structures, thromboembolism and spontaneous rupture. DAA has also been demonstrated in utero by fetal echocardiography. Studies have shown there may be a strong correlation between patients with connective tissue disorders like Marfan and Ehlers-Danlos syndromes and a ductal aneurysm.
DAA in newborns is usually asymptomatic, but can present with symptoms of a murmur, cyanosis, stridor, respiratory distress and a weak or feeble cry. On chest x-ray a prominent ductal “bump” can also be seen. It’s common for ductal aneurysms to resolve spontaneously, so symptoms can be transient. Case studies have described the spontaneous regression and natural resolution of DAA in patients that are asymptomatic as passing through stages of compression, septation/loculation, thrombus formation and eventual resolution (see image 1). Surgical repair may be necessary if there is significant compression or concern for possible rupture.
Optimal Echocardiographic Views:
Echocardiography is the modality of choice for ruling out a DAA, however X-ray, CT and MRI can add valuable information and help diagnose a DAA.
The best views by echocardiography are high left parasternal and suprasternal views. An unusual direction of the PDA flow into the main pulmonary artery may be the first clue of a ductal aneurysm.
From a high left parasternal, short axis view, a DAA is identified as a large structure seen leftward and superior to the LPA and enters into the MPA. In this view three large vessels are seen from medial to left lateral position, the ascending aorta, MPA, and ductal aneurysm, deemed the “triple star sign” (see image 4 & 5).
In suprasternal notch short axis imaging, if you angle posterior to image the descending aorta you can see a classic “Rabbit ear sign”. The right sided ear is the transverse aortic arch and descending aorta and the left sided ear is the ductal aneurysm. (See image 4B).
Some structures that may mimic a DAA are; mirror image of the pulmonary artery, normal prominent ductal bump, a left SVC, dilated atrial appendage and a vertical ductus arteriosus. If a dilated and tortuous vascular structure is visualized protruding left of the aortic arch, a DAA must be excluded.