Supracardiac Total Anomalous Pulmonary Venous Return
Amna Qasim, MD
Overview and Natural History
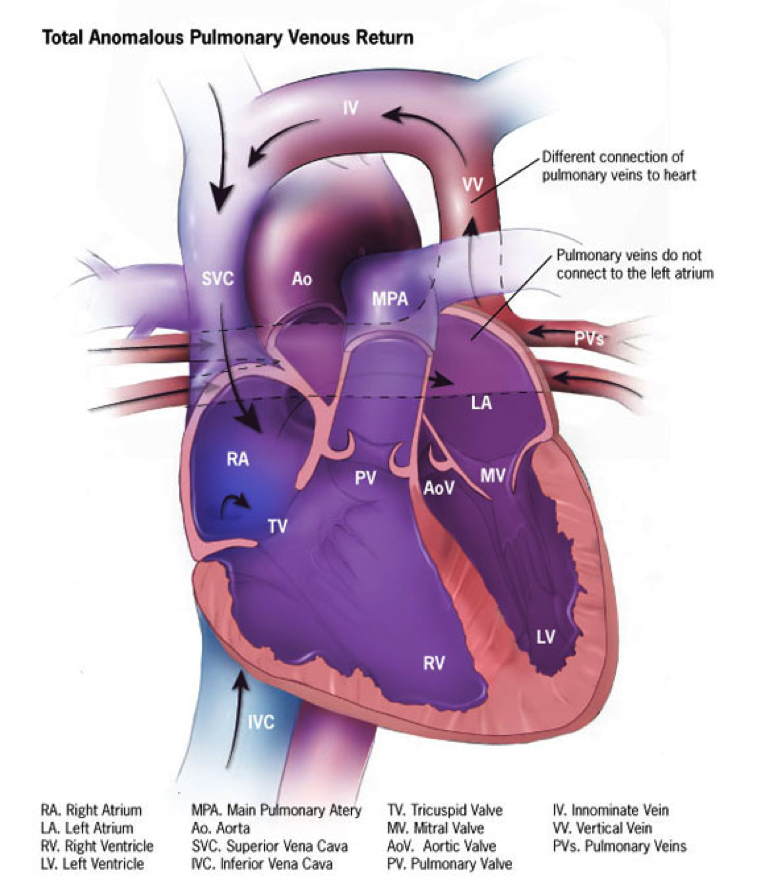
Total anomalous pulmonary venous connection is when all of the pulmonary veins returning from the lungs have an abnormal connection and drain anomalously to the right side of the heart instead of the left atrium. Supracardiac TAPVC is the most common type of anomalous pulmonary venous connection. In supracardiac TAPVC, the common pulmonary vein drains superiorly via a vertical vein into the left innominate vein, the right superior vena cava, or the right azygos vein by way of an ascending vertical vein.
Epidemiology
TAPVC has been described in 9 in 100,000 of the population. Supracardiac TAPVC is the most common type (47% in the largest published series) and in this group the most common site of connection is to the left innominate vein (36% of all cases).
Embryology and Genetics
In the human embryo, the primordia of the lungs, tracheobronchial tree and larynx are derived from the foregut. The pulmonary vascular bed is derived from the vascular plexus of the foregut, i.e. the splanchnic plexus. In the early stages, the pulmonary vascular plexus has no connection to the heart and shares routes of drainage of the splanchnic plexus (i.e. the cardinal and umbilicovitelline systems). By the end of the first month of gestation, the common pulmonary vein (the origin of which is controversial) connects the pulmonary venous plexus to the sinoatrial part of the heart. After this, the connection between the pulmonary venous plexus and splanchnic plexus involutes and the common pulmonary vein incorporates into the left atrium such that the individual pulmonary veins connect separately and directly to the left atrium. Anomalous pulmonary venous connection results from aberrancies during embryologic development. TAPVC (no connection of pulmonary veins to the left atrium) occurs when the common pulmonary vein fails to develop or becomes atretic early in development and pulmonary venous blood drains via collaterals from primitive connections between the splanchnic plexus and the cardinal or umbilicovitelline system of veins.
Genetic and syndromic associations include Cat eye syndrome, Heterotaxy syndrome (TAPVC most common with right atrial isomerism and PAPVC with left atrial isomerism) and Holt-Oram syndrome. A monogenic pattern of inheritance has been suggested. In a large Utah kindred, the gene for TAPVC was mapped to 4p13-q12.
Types
TAPVC is commonly classified into 4 types:
Type I: Anomalous connections at the supracardiac level
Type II: Anomalous connection to the coronary sinus
Type III: Anomalous connections below the diaphragm (infracardiac)
Type IV: Mixed type of connections
Supracardiac TAPVC can be further divided into two subtypes:
1. Connection to the Right SVC or Right Azygous vein: The pulmonary veins from each lung join to form a confluence posterior to the LA. An anomalous vessel originating from the right side of this confluence ascends, passes anterior to the hilum of the right lung, and enters the
posterior aspects of the right SVC. In a rare case, the right-sided ascending pulmonary venous vessel connects to the azygous vein.
2. Connection to the Left Innominate Vein (LIV): In this type (the most common type of TAPVC), the pulmonary veins from a confluence immediately posterior to the LA. A venous channel originating from this confluence traverses anterior to the left pulmonary artery (LPA), mainstem bronchus and aortic arch before joining the LIV proximal to its origin from the left jugular and subclavian veins. The LIV then joins the right SVC in a normal fashion. The ascending vein can infrequently pass between the left pulmonary artery and left main bronchus which can lead to extrinsic compression to pulmonary venous flow causing obstruction.
Hemodynamics
The hemodynamics depend greatly on the presence or absence of pulmonary venous obstruction and the size of the interatrial defect. Supracardiac TAPVC causes right-sided volume overload (with right ventricular dilation and hypertrophy) and pulmonary over-circulation (with various degrees pulmonary hypertension). Restriction of the interatrial communication not only increases pulmonary over-circulation but also diminishes systemic output. If the pulmonary veins are unobstructed, some patients may be asymptomatic at birth, about 50% will present in the first month with heart failure and the rest will present by the first year of life (most patients have heart failure by 6 months of life). The mortality of untreated patients is 75-85% by 1st year of life.
Goals of Echocardiographic Exam
- Identify each pulmonary vein and its connection site by 2D and color Doppler. Do not assume two veins from each lung; the number of individual pulmonary veins varies, and additional vein(s) with separate connection(s) to a systemic vein (e.g., left innominate vein, azygous vein, IVC, SVC) should be excluded. In supracardiac TAPVC, the connection between the vertical vein and the systemic venous system is frequently easily imaged from high parasternal short axis and suprasternal notch views.
- Follow each anomalously connecting pulmonary vein from its origin to its connection to the confluence or vertical vein from multiple views by 2D and by color Doppler sweeps.
- Interrogate each pulmonary vein by spectral Doppler and record mean gradients; interrogate by spectral Doppler and record mean gradient in every site where flow velocity accelerates and the lumen narrows by color Doppler.
- Interrogate the course of the vertical vein by 2D, color Doppler and spectral Doppler (measure and report maximum mean gradient and site of highest gradient) with good sweeps with close attention paid to sites of potential obstruction (such as when the vertical vein crosses between the LPA and left bronchus)
- Measure the diameters of each pulmonary vein (if possible to see by 2D) and the smallest diameter of the pulmonary venous confluence.
- Image the anatomic relationship between the pulmonary venous confluence and the left atrium.
- Rule out mixed drainage (additional pulmonary veins draining a systemic vein separately) and anomalous systemic venous connections
- Assess atrial septum, direction of atrial shunt, and evaluate for restriction to flow (color and spectral Doppler).
- Assess presence and degree of right ventricular volume load (TV annulus diameter; diastolic septal flattening; qualitative assessment of RV size; RV volume by 3D, if feasible).
- Assess for pulmonary hypertension with RV pressure by TR and PR jet velocities and by systolic septal configuration.
References
1. Allen Hugh D. DDJ, Shaddy Robert E.,, F FT. Moss and Adams' Heart Disease In Infants, Children, and Adolescents Including the Fetus and Young Adult. 8th ed: Philadelphia: Lippincott Williams & Wilkins; 2013.
2. Lai W. ML, Cohen M., Geva T. Echocardiography in pediatric and congenital heart disease from fetus to adult. 2nd. ed: John Wiley and Sons Ltd.; 2016.
3. NEILL CA. Development of the pulmonary veins; with reference to the embryology of anomalies of pulmonary venous return. Pediatrics. 1956;18:880-887.
4. Ferencz C, Rubin JD, McCarter RJ, et al. Congenital heart disease: prevalence at livebirth. The Baltimore-Washington Infant Study. Am J Epidemiol. 1985;121:31-36.
5. Rammos S, Gittenberger-de Groot AC, Oppenheimer-Dekker A. The abnormal pulmonary venous connexion: a developmental approach. Int J Cardiol. 1990;29:285-295.
6. Bleyl S, Nelson L, Odelberg SJ, et al. A gene for familial total anomalous pulmonary venous return maps to chromosome 4p13-q12. Am J Hum Genet. 1995;56:408-415.
7. BURROUGHS JT, EDWARDS JE. Total anomalous pulmonary venous connection. Am Heart J. 1960;59:913-931.
8. Image Credits: Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities.
9. Shah S, Singh M, John C, Maheshwari S. Supracardiac total anomalous pulmonary venous connection with a descending vertical vein. Pediatr Cardiol. 2009; Oct;30(7):1043-5.