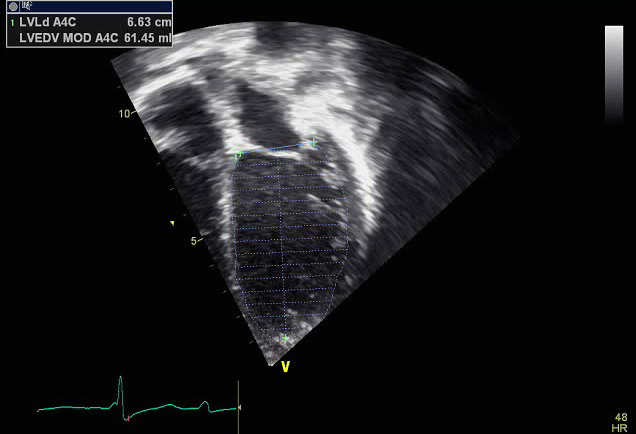
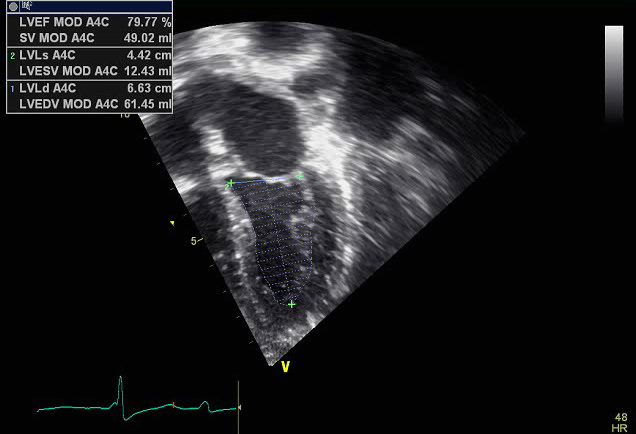
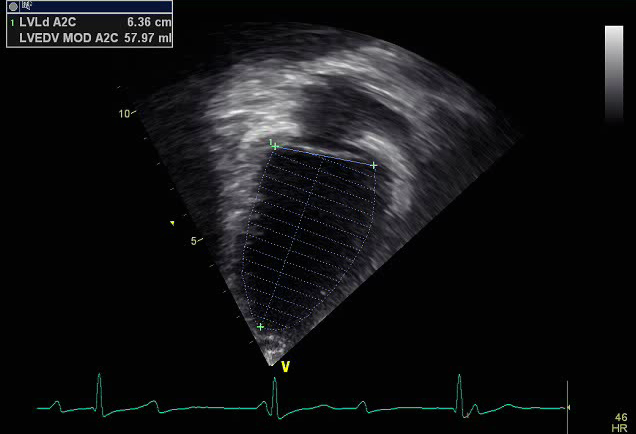
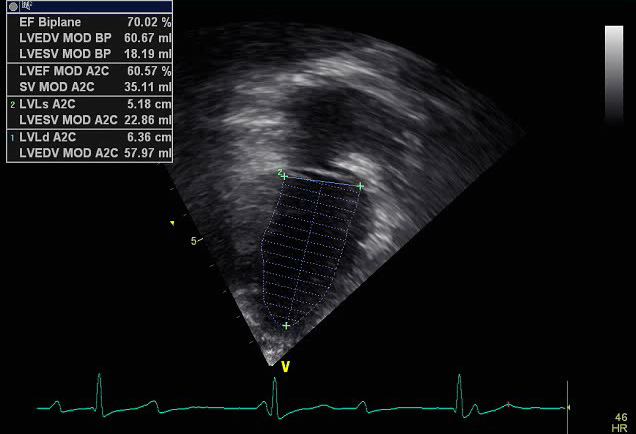
Ejection Fraction (Simpson's Biplane Method)
The left ventricle ejection fraction (EF) by Simpson's biplane method remains the best quantitative indice for the assessment of left ventricular systolic function. It divides the left ventricle into a series of elliptical discs (20 by convention), calculates cross sectional areas, and multiples by the length (height) for each disc to obtain volumes of cylinders. The sum of the volumes of the cylinders is the volume of the left ventricle. It is calculated by measuring left ventricular volumes from the apical four chamber and two chamber view at end systole and end diastole and using the following equation:
Ejection Fraction (EF) = (LV end-diastolic volume - LV end-systolic volume)/LV end-diastolic volume
- Normal: ≥ to 55%
- Mildly depressed: 45-54%
- Moderately depressed: 30-44%
- Severely depressed: <30%
How to Trace an Ejection Fraction
- Trace the endocardial border, excluding the papillary muscles
- Use end-diastolic and end-systolic frames determined by the maximum and minimum ventricular cavity sizes, not by the QRS ("biggest" and "smallest)
- Orthogonal planes- capture in true apical 4 and 2 chamber views (be careful not to foreshorten ventricles, particularly the apex)
Strengths of Ejection Fraction
- Less geometric assumptions so remains the most accurate quantiative marker to assess left ventricular systolic function
- Imaging endocardial borders usually good in children
- Can be improved with contrast agents
- Rapid and easy to do when image are accurate
Weaknesses of Ejection Fraction
- Still some reliance on geometric assumptions
- Limitations
- Load and heart rate dependent
- Dependent on normal LV geometry
- Need well defined endocardial borders
- High degree of user variation on:
- Where contours traced
- Truly orthogonal planes (inaccurate if left ventricle foreshortened from off axis views)
- Higher degree of inter and intraobserver variability

- Transducer placed on apical PMI (4th or 5th intercostal space)
- Midclavicular line and the apical PMI
- Notch at 3 o'clock
- Left ventricular systolic dysfunction